By Cristie Upshaw Travis
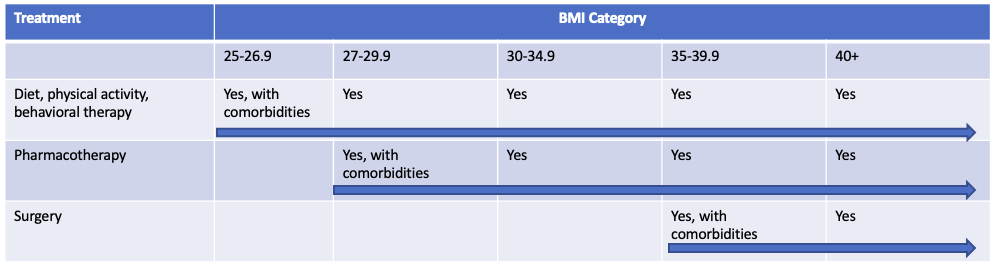
According to the American Heart Association, American College of Cardiology, and The Obesity Society, obesity management requires a “stepwise approach” (see chart).
Benefit design and coverage should align with clinical management to ensure that employees have access to the appropriate clinical services to maximize their opportunity to manage their obesity and be as healthy as possible for as long as possible.
In our historical work with MBGH employers as well as our 2020 focus on obesity and diabetes, we have learned that Memphis-area employers promote cultures of health and wellbeing that support diet, physical activity and behavior therapy. Extensive programs are generally available to support employees in starting and maintaining lifestyle changes. As you see above, these benefits and programs are critical for all levels of body mass index, even when paired with pharmacotherapy and surgery.
We have also found that Memphis-area employers generally cover weight management surgery, subject to significant pre-authorization requirements in order to maximize positive outcomes and lasting impact.
The gap for many Memphis-area employers is offering pharmacotherapy as a covered benefit. As the chart indicates, this management tool is best suited for those with a BMI starting a 27 if there are comorbidities and 30 if there are no comorbidities. Also note that pharmacotherapy can be continued for those that undergo surgery.
Results from a randomized trial of lifestyle modifications and pharmacotherapy treatment published in the New England Journal of Medicine in 2005, found that patients with both experienced approximately 2 times the weight loss of those with lifestyle modification alone.
A 2016 study published in Obesity Science and Practice (from the World Obesity and The Obesity Society) indicated that only 1% of the potential 1.8 million potentially eligible patients were receiving pharmacotherapy.
Average weight loss on anti-obesity medications ranges from 3-9%. Weight loss of 5-10% can result in reductions in type 2 diabetes, blood pressure, and blood lipid profile.
Unsure if you cover pharmacotherapy for your employees with obesity? Here are some steps you can take:
- Review your summary plan description and specifically the “exclusions” sections to see if you currently cover or exclude anti-obesity medications
- Examine your PBM contract, including provisions related to the plan design document and/or benefit specification forms. See if you have selected to cover or not cover therapeutic categories that include anti-obesity medications.
- Check out your pre-authorization requirements and, if you cover or decide to cover anti-obesity medications, check the box to include appropriate prior authorizations, which will reduce the likelihood that patients that do not clinically qualify will receive the medications.

Cristie Upshaw Travis, CEO
Memphis Business Group on Health
[email protected]
www.memphisbusinessgroup.org
