By Jill Berger
It’s no secret that the United States health care system is the most expensive in the world, though we trail behind most other developed nations on virtually every indicator of quality. This is enormously frustrating to employers, who pay for the majority of health care expenses in our country, with over half of U.S. citizens receiving coverage through an employer-sponsored health plan. How do employers get better care at a better price? Do health plans partner with employers to improve quality and reduce wasted costs?
As a former benefits executive myself, I struggled with these questions daily. In June 2020, The Leapfrog Group, an independent national health care watchdog organization, conducted a confidential online survey of executives of companies that administer and fund benefits for employees and/or dependents.
The purpose of the confidential survey was to gain employer perspectives on health plan effectiveness in achieving health care quality, safety and value. The survey asked a cross-section of American employers to identify which health plan(s) they contracted with and rate those plans on four key issues including:
- Responsiveness of the health plan to employer concerns;
- Transparency in helping employers and employees choose the best providers;
- Payment reform initiatives that incentivize excellence in the market; and
- Value strategies driven by health plans.
A total of 174 employers representing an estimated 4 million insured lives participated in the survey. Respondents cited their experience with health plans including Aetna, Cigna and UnitedHealthcare as well as a range of BlueCross and BlueShield (BCBS) plans, including Anthem and over a dozen state BCBS plans.
1. Responsiveness
Responsiveness is the foundation of an effective partnership between employers and health plans. The survey considered whether health plans understand employer goals and put a priority on improving employee health. While overall 58% of employers were satisfied with their health plans, they reported significant room for improvement in pursuing employer goals for quality and value.
Cigna earned the highest ratings from respondents for putting a priority on improving the health of employees, with 71% approval from those that identified Cigna as their health plan, while UnitedHealthcare and BCBS plans earned the lowest ratings, with 52% approval.
2. Transparency
Employers have long advocated for more information about the price and quality of health care services, which helps employees and other consumers make more informed decisions about their care.
Survey respondents offered discouraging ratings of health plan effectiveness in helping employees compare among providers. Employers reported a dismal 29% satisfaction level with their health plan’s transparency in comparing the quality of different hospital systems used by their employees. Though Aetna achieved the highest ratings for transparency, only 29% of respondents approved their performance. Just 13% of employers were satisfied with health plans’ transparency around quality and safety metrics.
3. Payment Reform
Traditional fee-for-service payment formulas pay providers a set rate for every service delivered, regardless of whether the patient needs or benefits from it. This creates perverse incentives to deliver more services even if they don’t equate to better care. As a result, employers are among the nation’s strongest champions of payment reform, including advancement of alternative payment models (APMs) such as bundled payments, centers of excellence, direct contracting, and value-based purchasing.
About a quarter of employer respondents reported using APMs; most survey respondents were not satisfied with health plans’ use of APMs. About a third of employers with Aetna reported satisfaction with APM deployment, compared with only one in five respondents with a BCBS plan.
4. Value
Employers expect plans to partner with them in the drive for value: cost-effective, high-quality care.
Just over half of the employer respondents agree that their health plan is on their side in reducing unnecessary health care costs. UnitedHealthcare was rated lowest among plans on this factor, with 43% of their employer clients satisfied. Employers are more satisfied with health plan efforts to advance health care quality, with 64% satisfied. Only 9% of employer respondents agreed that their health plan helped encourage Leapfrog Hospital Survey participation, a key employer initiative for quality and value.
Overall Grades
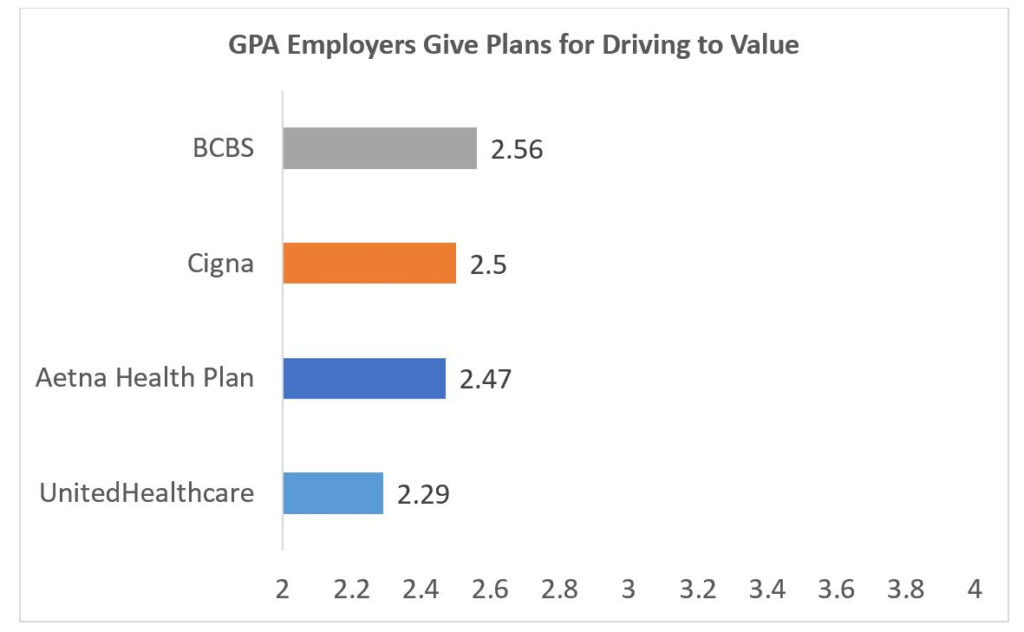
The final question asked of the employers was to grade their health plan, from A to F, on their ability to direct their employees to high-quality health care. Overall, employer respondents gave their plans a C-plus. The larger employers were tougher on the health plans than the midsize to small employers.
Summary
This survey brings into focus the conversations employee benefit executives need to have with their health plans. Employers in our survey see significant opportunities for improvement among national health plans in the movement for value in health care. While employers feel favorably toward their health plan in general, most are not satisfied with plans’ performances in galvanizing quality, value, and transparency in health care. Most do not perceive that health plans deliver the necessary tools to improve the quality and safety of care. Nor do the vast majority of employer respondents appear satisfied that their health plan puts their needs above the preferences of contracted providers, making it difficult for them to enact effective payment reform. A surprising number of employer respondents did not feel their plans offered adequate information for their employees to compare among providers.
Among the plans reported in the survey, Cigna was a clear leader in the movement for value. Employers gave UnitedHealthcare the lowest ratings for driving for value, reducing costs, and improving quality. Aetna led among plans for putting a focus on quality. However, no plan got an “A” grade from employers, which shows much room for improvement across the board.
Roadmap Forward
The survey should serve as a wake-up call to health plans. Employers are not convinced that plans are doing all they can to improve quality and cost-effectiveness. Health plans need to be more responsive to employer demands for improvements in health care.
Though the survey suggests that overall health plans lag in driving value, the good news is that the path forward is clear and well-paved. Over the past decade, employers collaborated with stakeholders on the regional and national level to expand tools and resources needed to advance quality and value. They removed many barriers to transparency and payment reform, and they built and tested initiatives that work. Health plans can and should take advantage of that progress and build on it. Leapfrog is among those offering well tested initiatives and tools to advance payment reform.
Ultimately, the most critical challenge identified by the survey would seem the most easily remediated. The vast majority of employer respondents did not believe their health plan put their needs first. In other industries, the customer comes first. In health care, however, too often there is confusion about the identity of the customer. So, let this survey reveal it: in the relationship between employers and health plans, employers are the customers because they pay the bills. As employers stand for quality of care and demand results for their investment in the health of their employees, they expect their health plan to stand with them. When that fundamental market dynamic is in place, better care and better value can cascade forward. Employers should expect nothing less.
Read Leapfrog’s full report outlining our employer survey findings on the organization’s website.
Jill Berger is the Director of Employer and Payor Engagement at The Leapfrog Group. Jill brings over 25 years of experience as a benefits executive for companies including GM and Marriott. She is an expert in managing employer benefits and developing innovative solutions for employers and health plans to transform health care.
